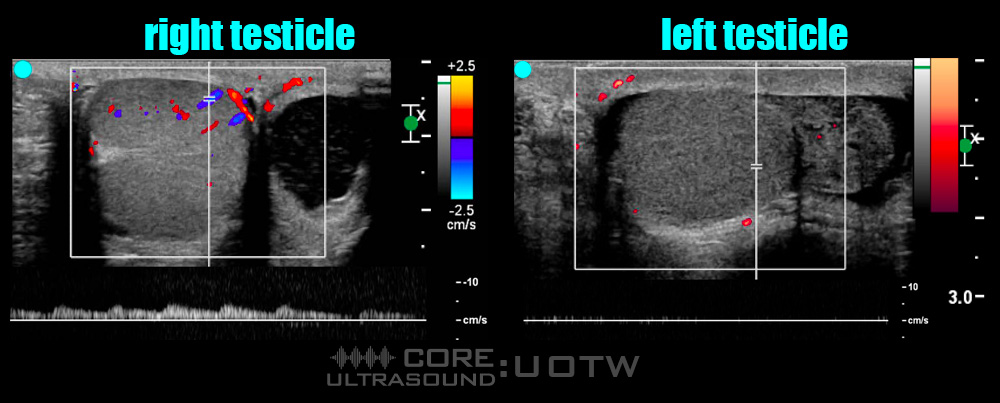
A 19 year-old-male presents to an emergency department with acute left testicular pain. It started acutely 3 hours prior to coming in. The patient is otherwise healthy. On physical examination, the patient does not have testicular swelling but his left testicle is tender to palpation. He has a cremasteric reflex present on the right side but not on the left. A bedside ultrasound is brought into the room and the following images are obtained:
What is the patient’s diagnosis?
Testicular torsion
Your bedside ultrasound shows absence of doppler flow in the left testicle, consistent with testicular torsion. Urology assesses the patient and agrees with your assessment. They performed a left testicular detorsion and a bilateral orchidopexy. The patient was discharged home the following day and his left testicle was salvaged.
- Testicular torsion is the result of spermatic cord twisting, which impairs blood flow to the testicles, leading to testicular ischemia and eventually necrosis if untreated1
- Torsion presents in a bimodal distribution, either very early in life in neonates, and in the early teenage to early twenties, often as a result of the bell clapper deformity of the tunica vaginalis.1
- Emergent urology consultation is required, as these patients require reduction of the torsed testicle for testicular salvage. Likelihood of testicular salvage is directly related to time from symptom onset to surgical treatment.2,3
- Classically taught physical exam maneuvers for testicular torsion such as absent cremasteric reflex, high-horizontal testicular lie, and scrotal erythema, edema, and swelling, are insufficiently sensitive and specific to rule in or rule out testicular torsion on their own.4
- Doppler ultrasound imaging is the most common form of imaging for patients with suspected testicular torsion, with lack of Doppler flow of the affected testicle specific for testicular torsion. 5,6
- However, this finding may be only 75% sensitive for testicular torsion, as false-negative studies may occur when a partially-torsed testicle is not tight enough to completely occlude arterial flow, or the testicle is intermittently torsing.7
- Spermatic cord twisting and spiralling, colloquially known as “whirlpool sign”, is the most sensitive and specific sign for testicular torsion in adolescents and adults, with a sensitivity of 92% and specificity of 99%.8
- For cases with a high index of suspicion for torsion, simultaneous consultation with urology while imaging the patient should be considered as time is testicle.
Author: Ben Forestell, MD and Sameer Sharif, MD FRCPC DRCPSC
Peer Reviewer: Jacob Avila, MD
References
- DaJusta DG, Granberg CF, Villanueva C, Baker LA. Contemporary review of testicular torsion: new concepts, emerging technologies and potential therapeutics. J Pediatr Urol. 2013 Dec;9(6 Pt A):723-30. doi: 10.1016/j.jpurol.2012.08.012. Epub 2012 Oct 6. PMID: 23044376; PMCID: PMC3566290.
- Mellick LB, Sinex JE, Gibson RW, Mears K. A Systematic Review of Testicle Survival Time After a Torsion Event. Pediatr Emerg Care. 2019 Dec;35(12):821-825. doi: 10.1097/PEC.0000000000001287. PMID: 28953100.
- Visser AJ, Heyns CF. Testicular function after torsion of the spermatic cord. BJU Int. 2003 Aug;92(3):200-3. doi: 10.1046/j.1464-410x.2003.04307.x. PMID: 12887467.
- Mellick LB. Torsion of the testicle: it is time to stop tossing the dice. Pediatr Emerg Care. 2012 Jan;28(1):80-6. doi: 10.1097/PEC.0b013e31823f5ed9. PMID: 22217895.
- Baker LA, Sigman D, Mathews RI, Benson J, Docimo SG. An analysis of clinical outcomes using color doppler testicular ultrasound for testicular torsion. Pediatrics. 2000 Mar;105(3 Pt 1):604-7. doi: 10.1542/peds.105.3.604. PMID: 10699116.
- Yagil Y, Naroditsky I, Milhem J, Leiba R, Leiderman M, Badaan S, Gaitini D. Role of Doppler ultrasonography in the triage of acute scrotum in the emergency department. J Ultrasound Med. 2010 Jan;29(1):11-21. doi: 10.7863/jum.2010.29.1.11. PMID: 20040771.
- Bandarkar AN, Blask AR. Testicular torsion with preserved flow: key sonographic features and value-added approach to diagnosis. Pediatr Radiol. 2018 May;48(5):735-744. doi: 10.1007/s00247-018-4093-0. Epub 2018 Feb 21. PMID: 29468365; PMCID: PMC5895684.
- McDowall J, Adam A, Gerber L, Enyuma COA, Aigbodion SJ, Buchanan S, Laher AE. The ultrasonographic “whirlpool sign” in testicular torsion: valuable tool or waste of valuable time? A systematic review and meta-analysis. Emerg Radiol. 2018 Jun;25(3):281-292. doi: 10.1007/s10140-018-1579-x. Epub 2018 Jan 15. PMID: 29335899.



